
Consequences of the Crisis
In addition to the tragic loss of life – more than 47,000 deaths[1] from opioid overdose each year– the medical, financial and operational costs to hospitals are staggering. As the opioid epidemic rages into its third decade, the health care needs of opioid-addicted patients continue to rise in complexity and cost. And hospitals often receive little or no payment for the care they provide.
Medical Harms
Five years ago, this disease was very uncommon for us. Now, it’s become so common that we can’t keep up.
– Serena Day, MD, cardiology fellow at The Ohio State University
From babies experiencing withdrawal from being exposed to opioids in the womb to long-term addicts suffering from debilitating infection or disease, nurses and doctors are caring for more, and sicker, opioid-addicted patients every year.
Endocarditis. Prior to the opioid explosion, endocarditis was an infection that generally affected older people with heart defects or an artificial heart valve. But as more prescription opioid addicts turn to heroin and other injectable drugs, endocarditis cases have skyrocketed driven by contaminated needles that introduce bacteria into the bloodstream.
The American College of Cardiology has reported that drug-related endocarditis admissions at one Ohio medical center increased by 436 percent from 2012–2017. Tragically, one out of four of the patients admitted in 2017 died[2].
click to enlarge
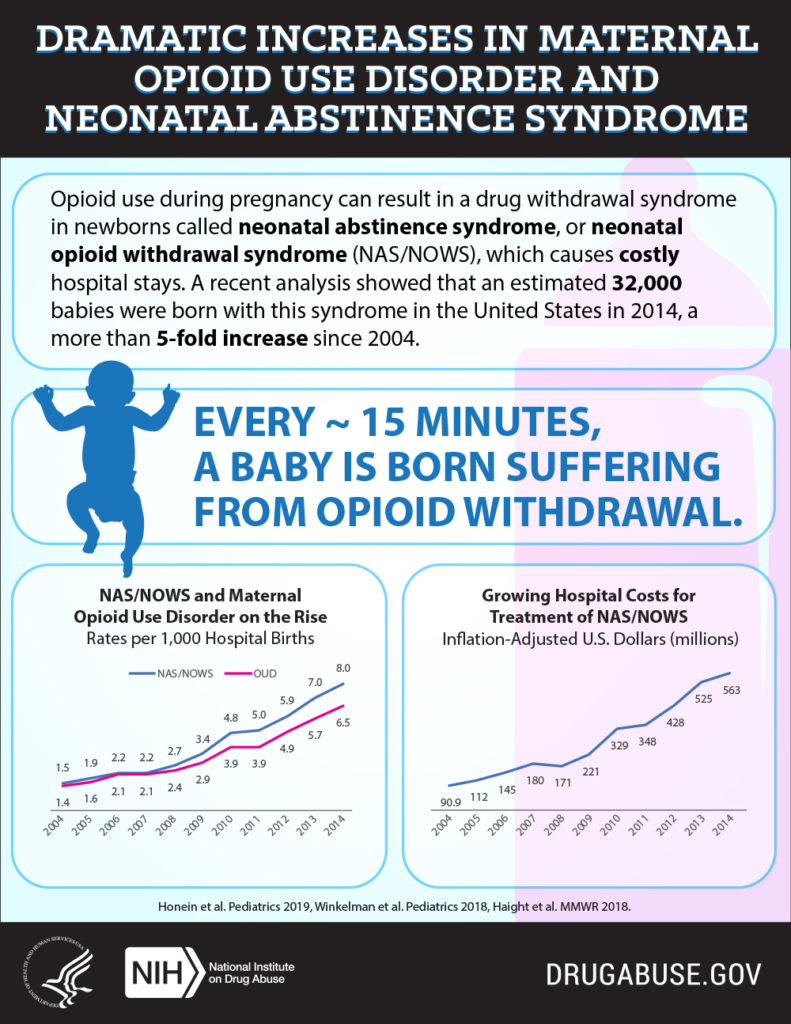
Neonatal Abstinence Syndrome. When a pregnant woman uses opioids, including prescription pain relievers, her baby is exposed to the drug and can develop NAS. These babies are born experiencing withdrawal symptoms such as tremors, seizures, trouble feeding, breathing problems and difficulty being consoled. Children who are prenatally exposed to opioids are about twice as likely to display intellectual disabilities and mild developmental impairments at the age of one.
The occurrence of NAS has become shockingly common in American hospitals: Every 15 minutes, a child suffering from opioid withdrawal is born[3].
The cost of caring for these vulnerable patients is staggering. One study documents national spending of more than $563 million a year on NAS deliveries and hospitalization[4].
Operational Realities
Nurses are in tears at the end of a shift.
Dr. Stefan Maxwell, neonatologist at CAMC Women and Children’s Hospital
Caring for opioid addiction and overdose patients now impacts nearly every corner of America’s hospitals.
Emergency Rooms have experienced growing levels of violence in the wake of this crisis. Hospitals have been forced to add security guards, cameras, metal detectors and increased visitor screening. They’ve invested in advanced drug-dispensing systems to prevent inappropriate access to prescription and hospital-strength pain medications. Some have built out treatment areas specifically for overdose patients and those experiencing the acute and chronic diseases that can result from opioid addiction.
The human toll on America’s hospital workforce may be the most significant consequence of the opioid crisis – and the most difficult to track. Human resource costs related to increased training, lost productivity, turnover, recruiting and workers’ compensation place a tangible drag on a hospital’s finances. But the emotional strain of caring for patients in crisis and the fear of violence in the workplace cannot be quantified.
Financial Challenges
It was compelling when we started seeing how much the hospital was billing [for endocarditis cases],” Bates said. “Over the last decade, there has been over $15 million in costs, and nearly $13 million of these costs went unpaid. This is a huge burden on the hospital and the community.
Mark Bates, MD, Director, Cardiovascular Fellowship Program & Researcher, Charleston Area Medical Center Health, Education and Research Institute
Hospitals are havens of community safety. They are required, by law, to medically screen and stabilize or transfer every patient with a medical emergency, regardless of the patient’s health insurance status or ability to pay.
That commitment to care comes with a significant price tag.
Health care costs related to the opioid crisis from 2001 to 2017 were estimated to have reached $215.7 billion[4] … and the annual expense continues to increase.
- The average cost to treat an overdose patient admitted to a hospital ICU was $92,408 in 2015[5].
- The costs to treat a NAS baby are three times greater than for a non-affected infant[6].
- Average cost for a hospital stay for drug use-associated infective endocarditis is $250,000[7].
Sources:
1 https://www.cdc.gov/drugoverdose/epidemic/index.html
2 https://www.cardiosmart.org/News-and-Events/2019/04/Opioid-Use-Causes-Dramatic-Rise-in-Life-Threatening-Heart-Infections
3 https://www.drugabuse.gov/related-topics/trends-statistics/infographics/dramatic-increases-in-maternal-opioid-use-neonatal-abstinence-syndrome
4 https://altarum.org/news/economic-toll-opioid-crisis-us-exceeded-1-trillion-2001
5 https://www.thoracic.org/about/newsroom/press-releases/resources/opioid-crisis-and-icus.pdf
6 https://www.ocregister.com/2018/12/27/born-on-drugs-babies-from-addicted-moms-are-increasing-at-an-alarming-rate-in-california/
7 https://acphospitalist.org/archives/2017/10/drug-associated-endocarditis.htm
